

Although the diagnosis can be made without pelvic films, pelvic radiographs are useful to assist in preoperative planning for restoration of the proper neck-shaft angle. The recommended views include the anteroposterior (AP) pelvis, AP and cross-table lateral of the affected hip and full-length radiographs of the affected femur. Plain radiographs are the initial films chosen to evaluate for these fractures. In type II fractures, the A subclassification describes a 3 part fracture with a separate GREATER trochanter fragment while the B subclassification describes a 3 part fracture with a LESSER trochanter fragment. The A subclassification in type I fractures is used for non displaced fractures while B fractures are displaced.

Type I is a 2 part fracture, Type II are 3 part fractures and Type III are 4 part fractures.
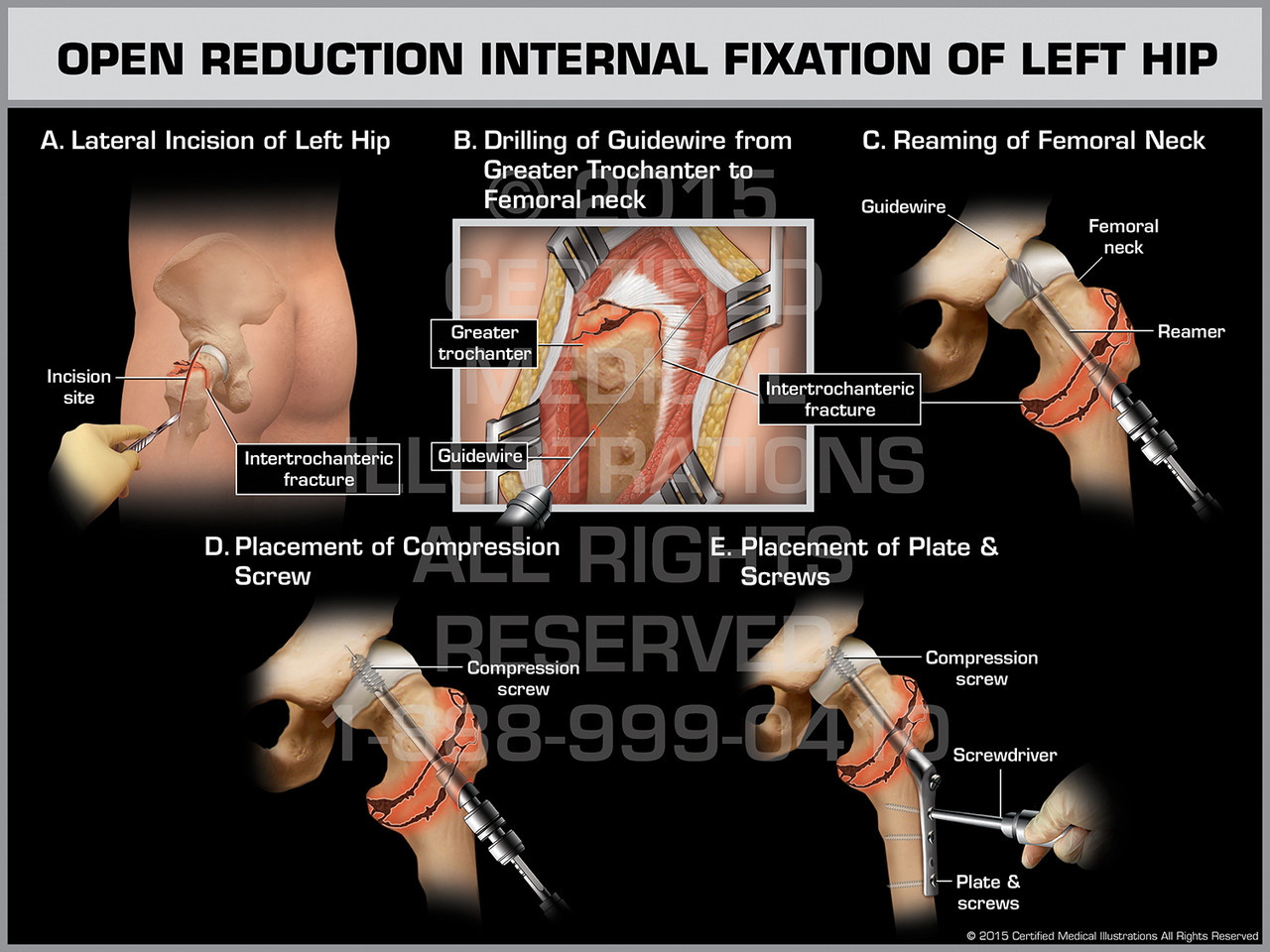
This Evans classification breaks down intertrochanteric femur fractures based on displacement, number of fragments and the type of fragment displaced. Examples of unstable fractures include: comminution of the posteromedial cortex, a thin lateral wall, displaced lesser trochanter fracture, subtrochanteric extension and reverse obliquity fractures. Stable fractures have an intact posteromedial cortex and will resist compressive loads once reduced. Determination of stability is important as it helps determine the type of fixation required for stability. These fractures are usually a result of a ground-level fall in the elderly population and are classified as either stable or unstable. Outcome studies indicate that conversion of Intertroch to THA is a less successful procedure, with higher rates of instability and greater troch pain, overall 88% survivorship at 10 years. Additionally, the fracture itself may have altered the anatomy of the proximal femur and thus increases the complexity of preparing the femur. The additional challenge of converting a failed Intertroch ORIF is an intertroch nonunion often requires a calcar replacing stem (about 65% of cases), and the stem must be long enough to bypass screw holes from the removed hardware which would otherwise act as stress risers. A screw and side plate is the preferred construct for the arthroplasty surgeon because removal can often be performed through the posterolateral approach used for the THA, and also because it preserves the abductor musculature. An intramedullary nail (hip IMN) is inserted through the abductor musculature and removal often causes further injury to the abductor complex, leading to postoperative limp and possible long term abductor deficiency and subsequent risk for instability. įailed Intertrochanteric Fracture ORIF (nonunion risk only 5%) is more complicated to revise. Outcomes suggest conversion failed femoral neck ORIF to THA is comparable to standard THA with 93% survivorship at 10 years (although possibly higher dislocation risk). Furthermore the femoral neck nonunion is excised with femoral preparation for the stem implant. Failed Femoral Neck ORIF (5-15% nonunion, 5-15% AVN) is often the easiest to convert to THA, as the standard treatment of 3 cannulated screws can be removed through the posterolateral incision for THA.


 0 kommentar(er)
0 kommentar(er)
